Radiation Therapy for Cancer Treatment at WVCI
Radiation therapy (also called radiotherapy) is a common treatment for cancer. About half of cancer patients receive radiation during their treatment journey. Radiotherapy can be used alone or in combination with other cancer treatments such as surgery, chemotherapy, and immunotherapy.

What is Radiation Therapy?
Radiation therapy uses high-energy beams or particles to kill or damage cancer cells. It plays an important role in treating certain cancers and easing cancer symptoms, including the treatment of lung, breast, prostate, and head and neck cancers.
X-rays, gamma rays, and charged particles are types of radiation used for cancer treatment. Radiation therapy kills cancer cells by damaging their DNA either directly or by creating charged particles (free radicals) within the cells that can, in turn, damage the DNA. When the DNA of cancer cells is damaged beyond repair, the cancer cells stop dividing or die. After damaged cells die, they are broken down and eliminated by the body’s natural processes.
What to Expect During Radiation Therapy Treatment
The cancer care team at WVCI will guide you through each step of the radiation treatment process, from initial consultation to follow-up care. These steps include:
- Consultation – Your radiation oncologist will meet with you to review your records and discuss your individual care plan.
- Simulation – Our staff will perform a CT scan and administer markings on your body to map out your treatment area.
- Treatment Planning – Your radiation oncologist will then determine the exact area of your body to be treated and the amount of radiation necessary.
- Radiation Treatment – Your radiation therapy will be administered over the course of two to eight weeks, depending on your treatment plan.
- Follow-up Care – Your doctor will provide details about how to care for the areas treated with radiation and any possible side effects. They will be available after your treatments have finished if you have any questions or concerns. As with all patients, your radiation oncologist is with you from diagnosis through survivorship and everything in between.
External radiation therapy sessions typically last 15-30 minutes. Most of the time is spent getting you into the exact correct position for treatment. The actual treatment takes five minutes or less. This is done on an outpatient basis and doesn’t often require a hospital stay. Because of the frequency of visits, finding a cancer center that’s close to you is ideal.
Types of Radiation Therapy
External Beam Radiation Therapy
External beam radiation therapy (ERBT) comes from a machine that aims radiation at your cancer. It does not touch you but can move around you, sending radiation to a part of your body from many directions. ERBT is a local treatment, meaning it treats a specific part of your body.
Hypofractionated radiation therapy is a more recent approach to external beam radiation therapy that gives the same dose of radiation over a shorter time frame. Instead of receiving radiation therapy for 6-8 weeks, the same results can be achieved in 4-5 weeks or less by giving a higher dose of radiation at each treatment session. Higher doses are possible because of the advanced technology available today that precisely aims the rays of radiation. This delivery method allows the cancerous cells to be treated with a higher dose while sparing nearby organs and tissues. Hypofractionated radiation therapy is currently used most often for breast, lung, and prostate cancers. The specific number of treatments needed depends on where the cancer is located, its size, and the patient’s overall health.
Types of External Beam Radiation Therapy Offered at Willamette Valley Cancer Institute
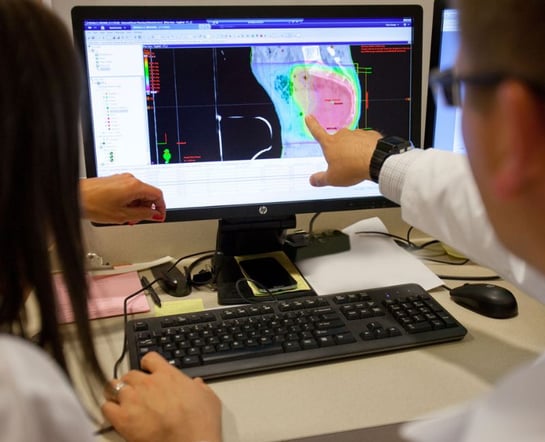
Several external beam radiation technologies are available through Willamette Valley Cancer Institute. The best option for each patient is determined by the radiation oncologist, who oversees the treatments and reviews the results with you and your medical oncologist.
3-Dimensional Conformal Radiation Therapy
Three-dimensional conformal radiation therapy (3D-CRT) uses images from CT, MRI, and PET scans to precisely plan the treatment area through a process called simulation. A computer program is used to analyze the images and to design radiation beams that conform to the shape of the tumor. The precise shaping makes it possible to use higher doses of radiation to the tumor while sparing normal tissue.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity Modulated Radiation Therapy (IMRT) is a type of 3-D conformal radiation therapy that uses CT scans or other three-dimensional images to build the treatment plan for the precise delivery of radiation. Like 3-D conformal radiation, radiation beams are aimed at the tumor from several directions. However, IMRT uses many smaller beams than 3-D conformal, and the strength of the beams in some areas can be changed to give higher doses to certain parts of the tumor. This enables a maximum dose to the tumor while minimizing the amount of radiation distributed to the surrounding healthy tissues.
- Volumetric-Modulated Arc Therapy (VMAT) or RapidArc® Radiotherapy is an advanced form of IMRT that allows a targeted, three-dimensional dose of radiation to be delivered directly to a tumor. The machine that delivers radiation can deliver the dose to the entire tumor in a 360-degree rotation, up to eight times faster than IMRT alone.
Image-Guided Radiation Therapy (IGRT)
Image-guided radiation therapy (IGRT) combines three-dimensional images, such as CT scans, with the precise technology of Intensity Modulated Radiation Therapy (IMRT) to pinpoint and treat cancerous tumors. During treatment, you will have repeated scans, such as CT, MRI, or PET scans, which are processed by computers to detect changes in the tumor’s size and location. The repeated imaging allows for your position or the radiation dose to be adjusted during treatment if needed. These adjustments can improve the accuracy of treatment and help spare normal tissue. IGRT is used to treat tumors in areas of the body that are prone to movement, such as the lungs, liver, and prostate gland, as well as tumors located close to critical organs and tissues.
Surface-Guided Radiation Therapy (SGRT)
Surface-guided radiotherapy is an external beam radiation therapy technique that uses advanced 3D technology to target cancer cells with high precision. Throughout treatment with SGRT, the surface of your body is continuously monitored in real-time, ensuring that the tumor’s position is accurately targeted with the radiation beams. SGRT will automatically pause if you shift out of position, which protects healthy surrounding tissue. The precision and safety of SGRT make it ideal for treating cancers located near vital organs.
WVCI also uses AlignRT by Vision RT to enhance the accuracy of SGRT. Advanced 3D stereo camera technology thoroughly tracks the skin's surface, ensuring precise radiation delivery to the tumor site with even more accuracy than SGRT alone. This technology allows patients to be treated in less time because the radiation is more effectively delivered to the targeted area.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery isn’t really a surgery, but rather the use of focused, high-energy beams to treat small tumors with well-defined edges in the brain and central nervous system. It may be an option if surgery is too risky due to your age or other health problems or if the tumor cannot safely be reached with surgery. In SRS, many small beams of radiation are aimed at the tumor from different directions. Each beam has very little effect on the tissue it passes through, but a precisely targeted dose of radiation is delivered to the site where all the beams come together. GammaKnife and CyberKnife® are two common types of stereotactic radiosurgery.
Stereotactic Body Radiotherapy (SBRT)
Stereotactic Body Radiotherapy (SBRT) is an advanced type of non-surgical radiation technology used to treat body tumors in locations such as the lung, liver, abdomen, spine, prostate, head, and neck.
The TrueBeam™ linear accelerator system from Varian Medical Systems is one of the latest advancements in SBRT. This system offers an exact radiation delivery method that surpasses previous capabilities. With its millimeter-scale beam shaping ability, the sophistication of TrueBeam makes it possible to deliver radiation from multiple angles with a precision that enables the sparing of surrounding healthy tissue. Speed, power, and precision define the TrueBeam system, enabling the treatment of cancers once deemed challenging due to their location. Its advanced capabilities are crucial in managing complex cases, particularly in breast, lung, prostate, head and neck, and colorectal cancers.
Stereotactic Radiation Therapy (SRT)
Stereotactic Radiation Therapy (SRT) is a type of external radiation therapy that uses special equipment to position the patient and precisely deliver radiation to a tumor. The total dose of radiation is divided into several smaller doses given over several days. Stereotactic radiation therapy is used to treat brain tumors and other brain disorders.
Internal Radiation Therapy
Internal radiation therapy, more commonly called brachytherapy, involves placing a temporary or permanent radioactive implant inside your body, in or near the tumor. The implant could be in the form of seeds, balloons, tubes, capsules, ribbons, wires, pellets, or needles. Most brachytherapy is put in place through a catheter, which is a small, stretchy tube. Sometimes, it is put in place through a larger device called an applicator. The way the brachytherapy is put in place depends on your type of cancer. Your doctor will place the catheter or applicator into your body before you begin treatment.
Brachytherapy makes it possible to position a higher total dose of radiation in a smaller area than what can be achieved with external beam radiation, resulting in less radiation exposure to surrounding healthy tissue or tissues that could be very sensitive to radiation. The amount of time the implants are in place varies by the patient and the type of cancer. Some patients have implants that are left in place for only a few minutes or a few days (high-dose-rate brachytherapy), while others have implants that are left in place to slowly break down on their own (low-dose-rate brachytherapy).
High-Dose Rate (HDR) Brachytherapy
High-dose-rate (HDR) brachytherapy delivers high doses of radiation to the tumor area from within the body or on the surface of the skin. It is administered through an applicator tube or thin catheter that is inserted into the body or through an applicator that sits on top of the skin.
This process delivers radiation for several minutes to the specific area where the cancer is located, sparing surrounding tissue. The radiation is removed from the body, unlike low-dose brachytherapy which may stay implanted.
- Endometrial Cancer HDR Brachytherapy is an endometrial cancer treatment that involves a source of radiation being placed into a cylinder and inserted into the vagina. The radiation mainly affects the area of the vagina in contact with the cylinder.
- Cervical Cancer HDR Brachytherapy is a cervical cancer treatment that involves delivering radiation to the cervical tumor from implants that are placed into the vagina and uterus.
- Skin Cancer HDR Brachytherapy is a non-melanoma treatment that involves placing the radiation source very close to the skin cancer for short periods of time. The Treatment course is shorter and more focused than external beam radiation, making it an ideal alternative to Mohs surgery for select small skin cancers.
Not all external brachytherapy is the same. HDR Brachytherapy, has been extensively studied and proven effective for treating non-melanoma skin cancer with excellent cosmetic and safety results when performed by a radiation oncologist. Electronic surface brachytherapy, also referred to as IG-SRT, is not well studied and is not recommended due to "insufficient long-term efficacy and safety data to support the routine use..."1
1. The NCCN Radiation Therapy CompendiumTM, Guidelines Version 1.2025, Squamous Cell Skin Cancer
Low-Dose Rate (LDR) Brachytherapy
Low-dose rate (LDR) brachytherapy delivers radiation using a radioactive device or implant placed inside the body. The device delivers a low dose of radiation to a limited area over a period of 20 to 50 hours. It is one of the most focused, precise forms of radiation therapy and spares much of the surrounding tissue. LDR can be used to treat various cancer sites, such as the prostate, uterus, or cervix.
* WVCI does not currently offer HDR Brachytherapy for prostate cancer at this time.
Related Reading:
Pros and Cons of Treating Cancer with Radiation Therapy
.jpg?width=710&name=Pros%20and%20Cons%20of%20Treating%20Cancer%20with%20Radiation%20Therapy%20(1).jpg)
Who is on Your Radiation Oncology Team?
When receiving care at one of our cancer centers at Willamette Valley and along the Oregon coast, you'll encounter several different people as part of the treatment planning and delivery process. Your team includes:
- Radiation Oncologist - this doctor oversees your radiation therapy treatments. These physicians work with the other members of the radiation therapy team to develop your treatment plan and ensure that each treatment is given accurately.
- Radiation Oncology Nurse - nurses who specialize in caring for patients receiving radiation therapy. They will work with the radiation oncologist and technician as well as help explain treatment, side effect management, and other important information to each patient.
- Radiation Therapist - the highly trained technologist who administers the radiation therapy to the patient over the course of their treatment plan.
- Physicist - specializing in cancer treatments, the physicist works with the radiation oncologist while planning each radiation treatment and any follow-up changes that may need to be made once the patient begins radiotherapy.
- Dosimetrist - the person who calculates the dose of radiation to make sure the tumor gets enough radiation but not more than is needed to reduce side effects for the patient as much as possible.
Did you know low-dose radiation therapy may help reduce pain and inflammation for individuals with osteoarthritis?
Willamette Valley Cancer Institute offers this non-invasive treatment to support better mobility and quality of life for arthritis patients in the Willamette Valley and the Central Oregon Coast at our Eugene location.
Choosing Willamette Valley Cancer Institute for Radiation
Radiation therapy for cancer treatment requires a high level of skill, precision, and experience. The radiation oncologists at WVCI use the latest technology and have the knowledge to ensure that all equipment is properly functioning and delivering radiation with extreme accuracy.
Our cancer centers have access to the newest and safest methods of radiation therapy treatment for patients throughout the Willamette Valley and the Oregon coast. When you’re ready, click the button to make an appointment with one of our radiation oncologists for personalized treatment planning at a location convenient to you in Eugene, Oregon.