When it comes to improving the outcomes for patients with lung cancer, advances in treatment are important. And so is detecting the disease early.
In 2015, two significant breakthroughs happened: Medicare instituted coverage of lung cancer CT screening for those considered high-risk. And significant steps were made in the development of immunotherapy drugs.
“We’ve spent the last 20 to 30 years figuring out ways to kill rapidly dividing cancer cells,” says Willamette Valley Cancer Institute medical oncologist Dr. Matthew Lonergan. “We’ve now begun to figure out the pathway of immunosurveillance and how cancer cells escape the immune system.”
Newest developments
Last year, the FDA approved two checkpoint inhibitors for the treatment of non-small cell lung cancer, which accounts for about 85 percent of lung cancer cases: Opdivo (nivolumab) and Keytruda (pembrolizumab). Both inhibit an immune checkpoint called PD-1 and are approved for patients with non-small cell lung cancer who have stopped responding to chemotherapy.
“It was discovered that cancer cells have a protein coating that essentially makes them invisible to the immune system,” says Dr. Lonergan. “This new group of therapies inhibits the protein and uncloaks the cells so the immune system can identify them as foreign and kill them.”
The drugs are given intravenously every 2-3 weeks and are not as toxic to the body as chemotherapy. Not all metastatic lung cancer patients respond to immunotherapy, but in those who do, prolonged survival has been significant.
“There is a group of people who derive a benefit of two to three years of additional survival from this therapy, as opposed to getting two to three months—20 percent of people get two years and maybe longer,” says Dr. Lonergan.
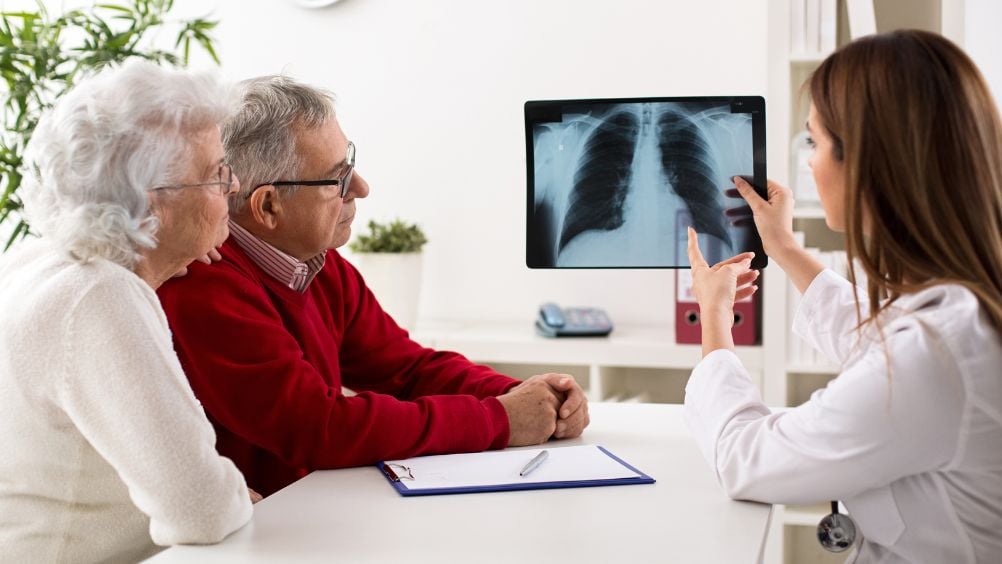
Detecting lung cancer earlier
CT scans are currently the only approved way to screen for lung cancer. This imaging test can detect it in the early stages, when the disease is most treatable. According to the National Cancer Institute’s National Lung Screening Trial in 2011, yearly low-dose CT scans have reduced lung cancer deaths among high-risk patients by 20 percent.
That’s why, last year, the Centers for Medicare and Medicaid Services adopted protocol to pay for lung cancer screening with a low-dose CT scan for those who qualify under current screening recommendations:
• Are 55 to 77 years old
• Are smokers or past smokers who quit within the past 15 years
• Have a smoking history equivalent to a pack a day for 30 years
• Show no signs or symptoms of lung cancer
• Are healthy enough to tolerate treatment for early-stage lung cancer, if needed
“With technology like imaging and radiation interventions, we can treat smaller and smaller tumors with more accuracy,” says WVCI radiation oncologist Dr. Haidy Lee. “For the most part, when lung cancer is caught early, it’s typically by accident. It’s usually found when a patient gets a CT scan for other reasons. But we want to catch lung cancer early, which is why screening is becoming an increasing topic of discussion among health care providers.”
There is an ongoing discussion in the medical community over the effectiveness of lowering the screening age even further, to age 50. But there’s also concern that screening more people at a younger age will result in more false positive results.
“We accept a certain amount of false positives in screening—screening isn’t 100 percent accurate,” says Dr. Lee. “But the goal is to catch more cancers at an earlier stage. That’s the trade off.”
A promising future
For those already diagnosed with late-stage lung cancer, hope lies in the developing field of immunotherapy. While oncology research is still a long way from a cure for metastatic lung cancer, oncologists are optimistic that new treatments will help their patients enjoy longer, more comfortable lives.
“The next five to 10 years are going to be really exciting,” says Dr. Lonergan. “The fact that these therapies worked in a place where we didn’t expect them to work five or seven years ago, I think there’s probably a whole series of therapeutic molecules and therapeutic infusions that will come out in the next five years that will hopefully build upon these two drugs for a multitude of cancers.”