Pictured above: Linn Bergander, PA-C, MPH; Aaron Wilson, RN Robot Charge Nurse; Erin Millard, RNFA; Payden Tanner, CST; Kathleen Yang, MD; Luosong Stratton, CST; Sara Opolka, RN; Carmen Reveal, CAN; Charles Anderson, MD; Brian Bourdage, da Vinci representative; and Martha Espinosa-Blank, CRNA
Kathleen Yang, a gynecologic oncologist at Willamette Valley Cancer Institute, is the first female surgeon in the state of Oregon to achieve a milestone—she performed her 1,000th surgery using robotic technology called the da Vinci Surgical System.
“This technology has drastically changed the way we practice medicine and has enhanced the patient experience,” says Dr. Yang. “It’s shortened the length of time a patient is hospitalized, while improving their recovery time.”
The FDA approved the da Vinci technology for gynecologic surgeries in 2006. Yang and her WVCI colleagues Dr. Charles Anderson and Dr. Audrey Garrett are the only gynecologic oncologists on the I-5 corridor between Sacramento and Portland using this technology. Between them, the oncologists have performed nearly 3,000 surgical procedures.
“More than 90 percent of the robotic cases I do, and certainly the most challenging surgeries, are performed on patients at Sacred Heart Medical Center at RiverBend,” Dr. Yang says. “The other 10 percent of surgeries are done at Good Samaritan Regional Medical Center in Corvallis and McKenzie Willamette Medical Center in Springfield.”
How does robotic surgery work?
The da Vinci surgical system features a magnified 3D high-definition camera and tiny wristed instruments that bend and rotate far greater than traditional laparoscopic instruments, enabling surgeons to operate with enhanced vision, precision, dexterity and control. The system cannot be programmed or perform in any way without the surgeon’s input. “It’s important for patients to know that the procedure is done by their surgeon, not the robot,” says Dr. Yang.
Benefits to the patient
The advantages of robotic technology for both the surgeon and the patient are dramatic. It allows Dr. Yang to treat her patients through just a few small incisions, while maneuvering the surgical tools in a way that is more gentle on the body.
“That means there is less scarring, reduced pain, a lower risk of complications or infection—and patients are able to go home sooner and recover faster than with traditional surgery,” Dr. Yang says.
Often, patients are released from the hospital the same day they have the procedure, instead of spending 3-5 days in the hospital, which is the standard following traditional open surgery. Patients also report being able to recover in one to two weeks with robotic surgery, instead of six to eight weeks.
In addition to treating gynecologic cancers, the da Vinci robotic surgery system is used in cardiac, colorectal, bariatric, urologic, thoracic, and head and neck surgery. For the gynecologic cancer team at WVCI, it has been a game-changer in treating uterine, cervical and ovarian cancers, especially complex cases.
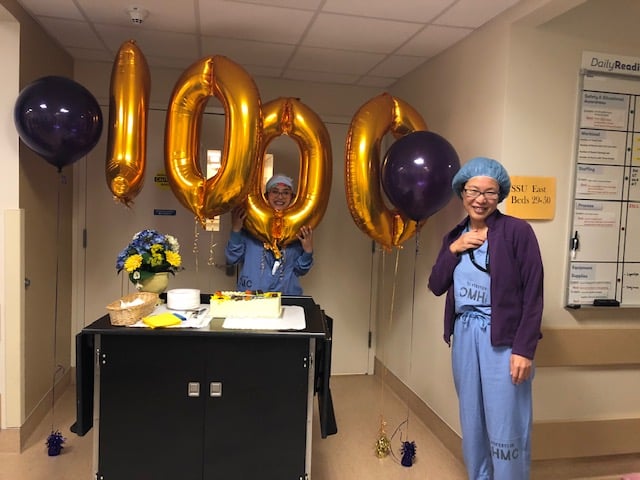
Dr. Kathleen Yang is the first female surgeon in Oregon to complete 1,000 robotic surgeries.



